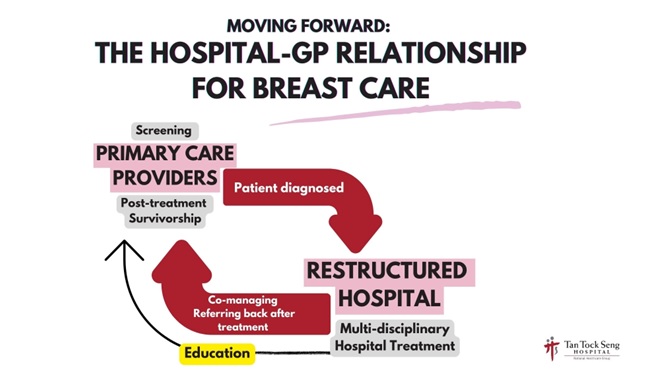
Traditionally, women would go to their primary care providers, such as general practitioners (GPs) or at polyclinics, to get their breast screening and examination. If necessary, cases with further examinations needed will be referred to the care teams in acute hospitals.
In Tan Tock Seng Hospital (TTSH), the majority of cases seen by the Breast Clinic are referred by GPs or polyclinics. These patients would undergo further assessment if required and embark on their breast cancer journey if diagnosed – this includes consultations, surgery, further adjuvant treatment such as hormonal, radiotherapy or chemotherapy, and physiotherapy sessions.
At this point, more often than not, there would be no further interactions between patients and their primary care providers.
How can our GPs support the load taken on by the hospital - and at the same time upskill on their capabilities and expertise to play a greater role for patients who require breast care?
In June 2024, TTSH and National Healthcare Group Polyclinics (NHGP) organized its first workshop for GPs attended by about 20 primary care physicians. Titled 'BREAST 101: Managing Common Breast Conditions and Understanding Breast Cancer', TTSH's breast care team – including breast cancer surgeons, radiologists and medical oncologists - shared with the attendees on the breast screening process, the updated referral framework, the challenges faced by breast cancer patients and survivors, as well as support measures that can be rendered to them in their survivorship journey.
During the session, the participants engaged the presenters with questions on how they could further develop their skills to provide more meaningful care for the patients and debunked several fears or misconceptions regarding breast conditions. They were also broken up into smaller groups to have more focused discussions on case studies, which were modeled after actual patient conditions.
Some responses from our participants
"What has been most helpful? Collaborative care. Given me knowledge and confidence when I encounter patients with breast conditions. Understanding of the imaging and management of breast cancer. Learning about background processes was useful."
"Many enjoyed the course and hope it could be scaled up to benefit all GPs and incorporated into the CFPS FPS course for primary care physicians."
Why is it important that our primary care providers be involved in the fight against breast cancer?
The best way to prevent breast cancer is to go for early and regular screenings. However, according to the latest National Health population health survey, only about 37.6% of women aged 50-69 in Singapore are actively going for mammograms - a significant contrast from Western counterparts with about 50% to 80% mammogram rate among women of the same age group.
There are many factors that could lead to women avoiding mammograms altogether. It could include the fear of diagnosis or death, the worry of medical bills from treatment, or they could simply be uneducated on the issue altogether. Our primary care providers are more entrenched within our communities and neighborhood housing estates - that patients are more likely to visit their primary care doctors more often than a specialist in an acute hospital.
The trust and relationship built between a GP and their patient could be the key to getting them to be more informed and proactive in knowing more about the health and management of their breasts. With our GPs being skilled in managing more aspects of breast care, it is more likely that these patients would be more comfortable to seek treatment regarding their breast health.
This would allow fewer women to fall through the cracks and be victims of untreated - or worse - undiagnosed breast cancer.
Furthermore, healthcare professionals in acute hospitals, such as the TTSH Breast Clinic, can then focus on more specialised care and intervention for these patients, or patients who are more severely ill.
At some point of time after treatment we also will want to return patients back to the care of their primary healthcare physicians to facilitate their chronic care. Many primary care physicians are also keen to continue follow up of their own patients after acute cancer treatment is complicated. Ongoing initiatives with our colleagues to involved them in the cancer treatment with this aim in mind is already in discussions and we hope to present these new initiatives in the near future.
From the Ministry-initiated HealthierSG enrolment, to more regular Mammobus deployments, many initiatives have been rolled out to encourage more women to step forward and go for early breast screening. Involving our GPs as a significant part of the breast care ecosystem is another significant step in reaching the ultimate aim.
Together with our patients and all health partners, we can help to improve the outcomes of breast cancer in Singapore.






