
Prime Magazine October/November Issue
Sugar Overload
Understanding More About Diabetes Mellitus
Diabetes mellitus (also known as diabetes or DM) is a condition where your body cannot manage sugar properly, resulting in high blood sugar (glucose) levels. In Singapore, one in three Singaporeans is at risk of developing diabetes, while about one in 10 Singaporeans have diabetes. Poorly controlled diabetes, high blood pressure and high cholesterol levels can result in health complications and damage to various organs, such as the brain, eyes, heart and kidneys (see Figure 1).
 Figure 1: Diabetes-related complications due to poorly controlled DM, high blood pressure and high cholesterol levels.
Figure 1: Diabetes-related complications due to poorly controlled DM, high blood pressure and high cholesterol levels.
Therefore, it is important to be aware of the significance of good diabetes control and the ways to manage it. Although diabetes is a chronic condition that has no cure, it can be well controlled through healthy eating, physical activity and medications. In other words, people with diabetes can be healthy too. Together, we can proactively take charge of our health and take diabetes medications as prescribed.
TYPE 1 AND TYPE 2 DIABETES
There are two main types of diabetes - Type 1 diabetes and Type 2 diabetes. In people with Type 1 diabetes, the pancreas makes little or no insulin. This form of diabetes is an autoimmune disorder, meaning the immune system mistakenly destroys its own beta cells in the pancreas. The beta cells are eventually destroyed, and treatment with insulin injections is necessary.
Compared to Type 1 diabetes, Type 2 diabetes is the more common subtype. It is a condition where blood glucose levels rise to unhealthy levels due to the body’s inability to use insulin effectively to take glucose into the body’s cells. This is also known as insulin resistance.
Further to Type 1 and Type 2 diabetes, pre-diabetes refers to blood sugar levels that are higher than normal but not high enough for a person to be diagnosed with diabetes. Having pre-diabetes puts you at an increased risk of getting Type 2 diabetes. Lifestyle changes, such as healthy eating, physical activity and weight loss, can delay the progression of diabetes or reverse pre-diabetes.
TIPS ON A HEALTHY LIFESTYLE
Healthy eating and physical activity play an important role in diabetes management. Exercise helps to keep us fit, reduces stress, and improves emotional well-being. You should aim to achieve healthy weight loss by balancing your physical activity and food intake. Eating well helps with your diabetes control, and your maintenance of a healthy weight, blood pressure and cholesterol levels. Here are three key healthy eating tips for a healthier you:
- Aim for regular meals at similar timings each day and avoid skipping meals.
- Consume two servings of fruits and two servings of vegetables per day. Do not take two servings of fruit at one go.
- Limit intake of food and drinks containing sugar, such as sweetened beverages, fruit juices, cakes, kuehs, desserts, chocolates, ice cream, etc.
Medications to Manage Dianetes
To better understand how medications work to control blood glucose levels, it is important to first understand the concept of insulin. Insulin, a hormone produced by the pancreas in our body, allows our body to use glucose for energy. The role of insulin is described in Figure 2.
- Insulin is a hormone that helps control the blood sugar level in our body.
- Insulin is made by beta cells in the pancreas in our body.
- Insulin acts like a key to unlock the door for glucose (sugar) to enter cells and by doing so, provides energy for the body and lowers the amount of glucose in your bloodstream.
Figure 2: Insulin acts like a key to unlock the door for sugar to enter cells and lowers the amount of sugar in your bloodstream.

When the pancreas cannot produce enough insulin or the body cannot utilise insulin effectively, blood glucose level remains persistently higher than normal. Therefore, insulin injections and diabetes medications that affect insulin release and insulin effect are a mainstay of pharmacological treatment for diabetes.
Besides oral tablets, insulin injections and non-insulin injectables may also be prescribed in combination to lower blood glucose levels and improve diabetes control. Another class of diabetes medicines are the Glucagon-like peptide-1 (GLP-1) receptor agonists. These medications work to slow digestion and absorption of sugars in the intestines.
Different medications work on different parts of the body to control blood glucose levels. Figure 3 shows medications prescribed for diabetes control and how they work. Some of these medications help to reduce insulin resistance (metformin, pioglitazone), while others help to remove sugar from the body (dapagliflozin, empagliflozin). There are certain medications which help by increasing the body’s natural response to sugar from food (linagliptin, sitagliptin), while there are also others which increase the release of insulin from the pancreas (glipizide, gliclazide, glimepiride, tolbutamide).
Figure 3: Different medications work on different parts of the body to control blood glucose levels.
Besides oral tablets, insulin injections and non-insulin injectables may also be prescribed in combination to lower blood glucose levels and improve diabetes control. Another class of diabetes medicines are the Glucagon-like peptide-1 (GLP-1) receptor agonists, such as dulaglutide, liraglutide and semaglutide. These medications work to slow digestion and absorption of sugars in the intestines. Additional benefits of this class of GLP-1 receptor agonists include weight loss, lowering the risk of heart disease, and slowing the progression of kidney disease.
As discussed earlier, insulin works by increasing glucose uptake into the cells in our body, lowering the glucose in the bloodstream. People with Type 1 diabetes (with little or no insulin) will require insulin injections in their diabetes treatment. As for Type 2 diabetes, it is a progressive disease, and some people with this form of diabetes may require a combination of oral tablets, insulin injections and non-insulin injectables to improve diabetes control.
There are different types of insulin injections available. They include:
- Basal (long-acting background) insulin,
- Bolus (short-acting mealtime) insulin, and
- Premixed insulin (combination of long- and short-acting insulin mixed into one product).
Discuss with your doctor or diabetes healthcare team on which is the most suitable for you.
For persons on regular insulin treatment and certain oral diabetes medications (i.e., sulfonylureas, such as glipizide, gliclazide, glimepiride and tolbutamide), it is especially important not to skip or delay meals in order to prevent the risk of hypoglycaemia (low blood glucose level).
Understanding Blood Glucose(BG) Levels and HbA1c
It is important to differentiate between blood glucose (BG) levels and HbA1c. BG refers to the amount of glucose in the blood vessel. BG level can be measured at the clinic during health screening, or when using a blood glucose monitoring machine (glucometer) at home. In contrast, HbA1c tells you about your diabetes control based on your average BG level over the past 2-3 months. It measures the sugar (glucose) attached to your red blood cells. The higher the HbA1c, the greater the risk of developing diabetes-related complications.
There is a good correlation between the HbA1c result and the range of BG readings. To achieve good diabetes control, you will need to keep BG levels within the target range to reach your optimal HbA1c. Table 1 shows the correlation between BG level and HbA1c. Your HbA1c and BG targets should be individualised according to your health condition. Do discuss your HbA1c and BG goals with your healthcare team.
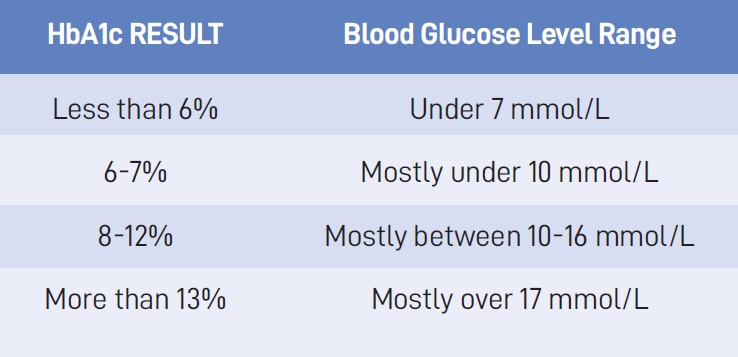 Table 1: HbA1c and correlation with blood glucose (BG) level.
Table 1: HbA1c and correlation with blood glucose (BG) level.
For medication-related or nutritional advice personalised to your medical condition, do speak to a healthcare professional, such as a doctor, pharmacist, dietitian or diabetes educator.
 *Acknowledgements and credits to: Ministry of Health Singapore National Diabetes Reference Materials Workgroup, National Healthcare Group DM Education Workgroup and NHG DM School.
*Acknowledgements and credits to: Ministry of Health Singapore National Diabetes Reference Materials Workgroup, National Healthcare Group DM Education Workgroup and NHG DM School.
Dr Lim Shu Fang is a Principal Clinical Pharmacist at Tan Tock Seng Hospital. Collaborating with endocrinologists and healthcare professionals in a team-based model, Dr Lim is actively involved in reviewing inpatients with diabetes during their hospital admission. In the outpatient setting, she conducts clinical review and education as a transdisciplinary Clinical Diabetes Educator during clinic consultation. Dr Lim is also the pharmacist representative in the Ministry of Health National Diabetes Reference Material and National Healthcare Group DM Education workgroups.
Tan Tock Seng Hospital